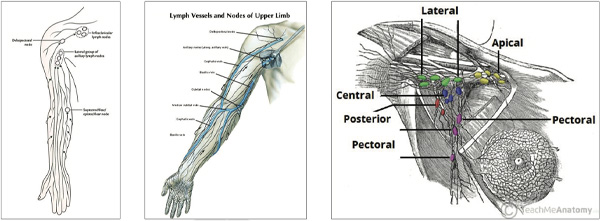
Breast cancer is still associated with high mortality rates and one of the most important factors governing long survival is accurate and early diagnosis. In underdeveloped countries, this disease frequently is only detected in advanced stages; however, through mammography, ultrasound breast and MRI mammography many women have been diagnosed at early stages. In this context, the sentinel lymph node (SLN) technique is associated with less postoperative morbidity compared to axillary lymphadenectomy. Lymphoscintigraphy has emerged as a method for the evaluation of lymphatic drainage chains in various tumor’s, being both accurate and noninvasive.
Through the years, the development of surgical techniques has made it possible to minimize deformities. The current trend is that to continue developing techniques that are as conservative as possible. SLN biopsy is prescribed in early tumor’s, avoiding unnecessary dissection of axillary lymph nodes.
Lymphoscintigraphy plays an important role in the identification of the sentinel lymph node, contributing to the prevention and minimization of postoperative complications. However, even with therapeutic changes, lymphedema remains a matter of concern.
There are several reasons for this. With the increasing survival, the limitations with which women will be obliged to live can cause psychological, physical, sexual and social issues; axillary lymph node preservation is indicated to tumor’s up to 3 cm and a clinically negative axilla. Although the detection of SLN reduces the incidence of lymphedema, it does not eliminate the risk of developing it, mainly those women with other risk factor such as obesity and previous anatomic alterations and; adjuvant treatments, particularly radiotherapy including drainage chains, remains an important risk factor for the development of lymphedema.
Lymphoscintigraphy shows that restoration of the original lymphatic pathway to the axilla after its initial disruption by nodal dissection was not uncommon and may prevent lymphoedema Studies found that regenerated lymphatic vessels and dermal backflow (the reflux of lymph to the skin) contributed to either restoration of the original pathway or rerouting of the lymphatic pathway to other regional nodes. Variation in the lymphatic drainage pathway and the mechanisms of fluid drainage itself are the foundation of new lymphatic drainage patterns considered to be significant in determining the severity with which lymphoedema develops
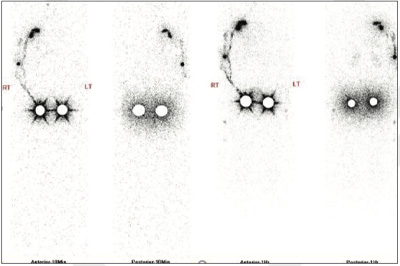
51 years old lady with history mastectomy and axillary lymph node dissection has lymphedema. Currently new onset of swelling, which is being resistant to compression.
REFERRED FOR UPPER LIMB LYMPHO-SCITNTIGRAPH
99m Tc – Nano colloid Lymphatic Scan of Upper Limb
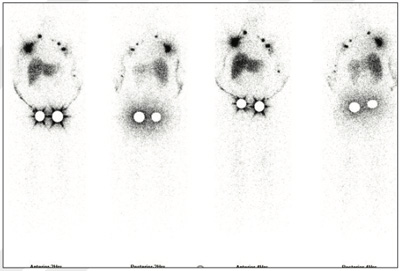
Subcutaneous tracer injection in between first and second finger on either side and subsequent image are obtained immediately, 1 hour, 5 hours, 2 hours and at 5 hours respectively.
No appreciable lymphatic drainage and non-visualisation of lymph nodes seen throughout the study.
Non obstructive lymphatic drainage pattern with well visualisation of axillary lymph nodes as well as epi-trocheal lymph node
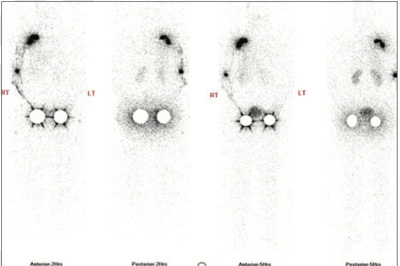
42 years old lady with history mastectomy and axillary lymph node sampling in 2017 (Cancer breast) , following which she had undergone adjunct chemotherapy and radiotherapy. C/o swelling in the right upper limb, which feels heavy and full.
REFERRED FOR UPPER LIMB LYMPHO-SCITNTIGRAPHY
99m Tc – Nano colloid Lymphatic Scan of Upper Limb
Subcutaneous tracer injection in between first and second finger on either side and subsequent image are obtained immediately, 1 hour, 2 hours and at 4 hours respectively.
Lymphatic drainage is overall non obstructive along with visualisation collaterals drainage approximately at the level of elbow region. Well visualisation of medial arm territory and axillary lymph nodes
Lymphatic drainage is overall non obstructive but relatively decreased and delayed (as compared to left side), which improves further on delayed images. Beside this there is slow tracer accumulation with stasis seen approximately in proximal half of forearm and at the elbow region. Well visualisation of medial arm territory, dorsal arm territory and axillary lymph nodes.
As compared to left side lymphatic drainage, the right side shows stasis of tracer retention in proximal forearm and elbow region, relatively slow and delayed drainage, which improves on delayed images, less tracer uptake intensity in axially lymph nodes (possibly due to decrease in reservoir capacity).
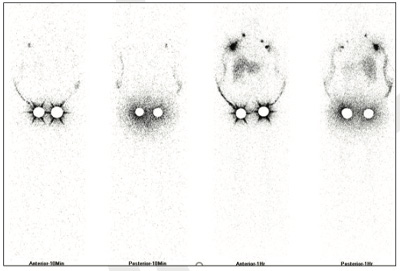
48 years old lady with history mastectomy and axillary lymph node sampling in 2018, following which she had undergone adjunct chemotherapy and radiotherapy. C/o swelling in the left upper limb.
REFERRED FOR UPPER LIMB LYMPHO-SCITNTIGRAPHY
99m Tc – Nano colloid Lymphatic Scan of Upper Limb
Subcutaneous tracer injection in between first and second finger on either side and subsequent image are obtained immediately, 1 hour, 2 hours, 4 hours and at 6 hours respectively.
Lymphatic drainage is overall non obstructive but relatively decreased as compared with opposite side. Visualisation of medial arm and axillary lymph nodes (except showing decrease in tracer uptake intensity as compared to opposite side, which is possibly to be due to decrease in reservoir capacity).
Lymphatic drainage is overall non obstructive. Visualisation of axillary lymph nodes with good tracer uptake intensities (good reservoir capacity).
Subcutaneous tracer injection in between first and second finger and subsequent images are obtained immediately, 1 hour, 5 hours, 2 hours and on either side at 5 hours respectively.
No appreciable lymphatic drainage and non visualisation of lymph nodes ( h/o axillary clearance) seen throughout the study.
Lymphatic drainage is non obstructive along with possible visualisation few collaterals are in elbow and upper arm region. well visualisation of axillary lymph nodes as well as epi trocheal lymph node.
Subcutaneous tracer injection in between first and second finger on either side and subsequent images are obtained Immediately, 1 hour, 2 hours and at 4 hours respectively.


Lymphatic drainage is overall non obstructive along with visualisation collaterals drainage approximately at the level of elbow region. Well visualisation of medial arm territory and axillary lymph nodes.
Lymphatic drainage is overall non obstructive but relatively decreased and delayed (as compared to left side) , which improves further on delayed images. Beside this there is slow tracer accumulation with stasis seen approximately in proximal half of forearm and at the elbow region.Well visualisation of medial arm territory, dorsal arm territory and axillary lymph nodes.
As compared to left side lymphatic drainage, the right side shows stasis of tracer retention in proximal forearm and elbow region, relatively slow and delayed drainage, which improves on delayed images, less tracer uptake intensity in axially lymph nodes (possibly due to decrease in reservoir capacity).
Subcutaneous tracer injection in between first and second finger on either side and subsequent images are obtained immediately, 1 hour, 2 hours, 4 hours and at 6 hours respectively.

Lymphatic drainage is overall non obstructive but relatively decreased as compared with opposite side. Visualisation of meadial arm and axillary lymph nodes ( except showing decrease in tracer uptake intensity as compared to opposite side, which is possibly to be due to decrease in reservoir capacity.
Lymphatic drainage is overall non obstructive. Visualisation of axillary lymph nodes with good tracer uptake intensities (good resevoir capacity).