Early diagnosis remains the best method of improving the odds of curing breast cancer. Among the tools currently widely available, screening mammography has been credited with an earlier diagnosis and a decreased risk of death from breast cancer. However, false negatives occur frequently, particularly when imaging post-surgical recurrence, fibrocystic breast disease and dense breast tissue in younger women. Mammography also has a low positive predictive value, and accurate second-line imaging methods are useful in some instances to reduce the number of unnecessary excisional biopsies.
Among the various imaging techniques used to assess primary or recurrent breast cancer, radionuclide imaging techniques such as planar scintigraphy , as well as SPECT-CT hybrid imaging can provide an accurate assessment of the presence and extent of disease as well as unique information about tumor biological characteristics such as the rate of proliferation and metabolic activity.
Several clinical studies in the medical literature have shown that 99mTc-MIBI, normally used for myocardial perfusion imaging, concentrates in breast cancers. This uptake is due to an increase in blood flow, number of mitochondria and cancer cell membrane hyperpolarization in the tumor and as a function of the expression of the multidrug resistance gene. 99mTc-MIBI scintimammography (SMM) has been used clinically to evaluate patients with a palpable breast abnormality when mammography is negative or indeterminate. The aggregated sensitivity and specificity of SMM in detecting a palpable primary breast cancer were, respectively, 85.2% and 86.6%. For non-palpable breast lesions, the sensitivity and specificity of SMM were 66.8% and 86.9%, respectively. Like magnetic resonance imaging (MRI) of the breast, Nuclear Medicine may also be helpful to determine if multiple breast tumors are present. For instance, a mammogram or ultrasound (sonogram) of the breast may reveal breast cancer in one area. However, a Nuclear Medicine breast imaging test may show that the cancer is in fact multi-focal; tumors are present in several areas of the breast. Determining the extent of breast cancer with Nuclear Medicine can help indicate treatment: breast conserving surgery (lumpectomy) or breast removal (mastectomy). Mastectomy is indicated if there are multiple tumors.
43 years old female.
Areas of suspicion in right breast upon physical examination.
Strong family history.
Mammogram findings: Extremely dense breasts. No suspicious masses or calcification.
Patient did not undergo biopsy and followed by the physician.
58 years old female.
Noticed swollen left breast three to four months ago.
sudden in onset, slowly progressive, mildly painful and redness over the skin.
No lump palpable/nipple discharge.
Similar complaints noticed in right breast two months ago.
Suspected and treated as bilateral mastitis.
Significantly dilated central sub-areolar ducts on either side (duct ectasia). No focal solid mass is seen. Normal sized right axillary benign looking lymph nodes with preserved fat hila noted.
Fairly well defined hyperdense lesion > 2cms in diameter is seen lateral and cranial to the level of right nipple shadow with another small lesion seen superficially above and lateral to right nipple shadow(corresponds to larger fibroadenoma and smaller intramammary lymph node.
Focal areas of abnormally increased tracer uptake seen in a) Larger one in upper quadrant of right breast. b) Smaller one diagonally above the larger one in right breast (Lesion a is metabolically more active than b).c) Upper quadrant of left breast, the tracer uptake intensity is much milder as compared to right breast abnormality (a) but looks like mirror image.
47 years old female. History of Total thyroidectomy (Histopathology- Papillary Ca thyroid (T1,N0,M0). Referred for 99mTc Sesatmibi whole body scan postoperative work up for residual thyroid tissue and metastasis.
Small residual thyroid tissue in thyroidal bed and focal area of intense uptake in Left breast(Accidentally).
61 Years old female. Strong family history of Ca breast.
Smooth bordered possibly benign calcifications are seen scattered over both the breasts.
56 Years old female with history of lump in right breast. Strong family history of Ca breast.
FNAC- Malignancy.
Ref for Isotope whole body bone scan for metastatic and staging work up.
99m Tc MDP Scintimammography (Done as out of interest) - Multicentric right breast lesions.
Whole body scan findings were unremarkable
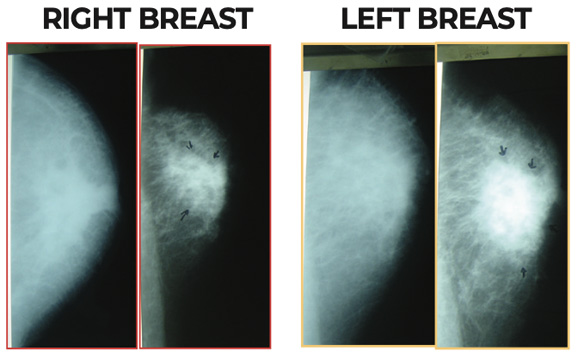
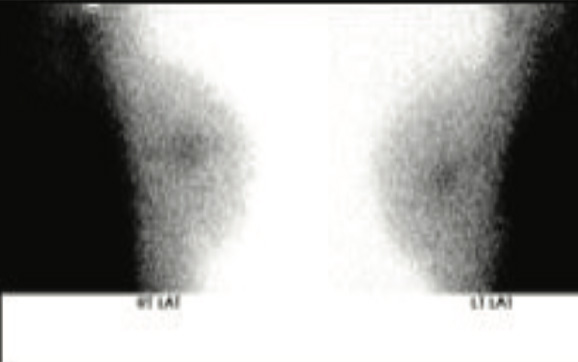
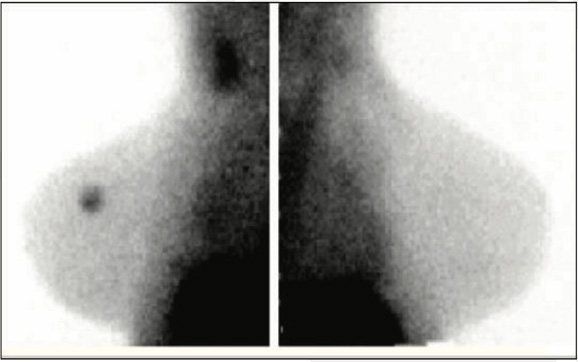
99mTc-methoxyisobutylisonitrile (MIBI) Scinti-Mammography (SMM) Showing a typical case of breast cancer in the external upper quadrant of the left breast.
Nuclear medicine breast imaging may be appropriate for patients with:
SMM is a nuclear medicine technique, which provides valuable, additional and complimentary information to that obtained by traditional anatomical screening and assessment. SMM can provide accurate and important information in women where x-ray mammography is difficult, equivocal or non-diagnostic.Helps the clinician to achieve a more accurate diagnosis and plan the treatment more efficiently. It provides answers to questions raised by mammography and help to reduce the stress and anxiety which patients feel when undergoing tests for breast cancer by providing an increased certainty of diagnosis.
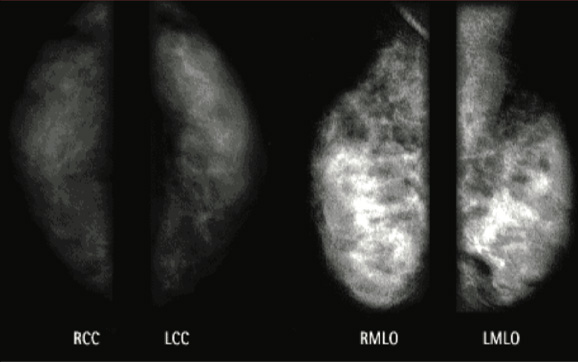
Case 1
Mammogram findings : Extremely dense breasts. No suspicious masses or calcification.
Case 1
SMM : No areas of increased focal uptakes.
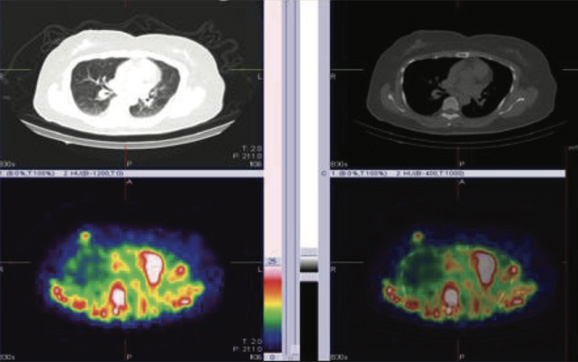
Case 2
USG BreastSignificantly dilated central sub-areolar ducts on either side (duct ectasia). No focal solid mass is seen. Normal sized right axillary benign looking lymph nodes with preserved fat hila noted.
Case 2
MammogramBilateral heterogeneous/inhomogeneous dense breast.No obvious speculated mass or suspicious clusters of micro-calcification. The nipple retracted.
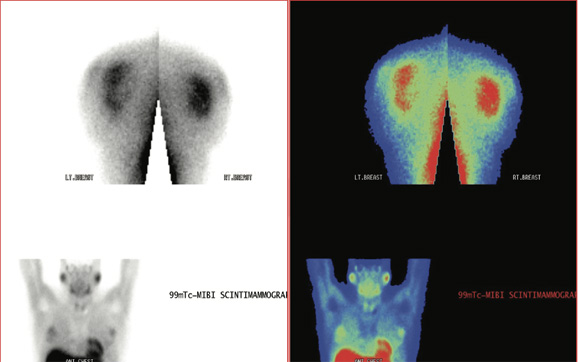
Case 2
SMM (Scintimammography)Fairly large diffuse area of abnormally increased tracer uptake seen in both the breast suggesting metabolically active abnormality. Biopsy is mandatory to exclude malignancy.
Bilateral US guided breast needle biopsiesInvasive duct carcinoma (NST): grade III: of both breast right and left.
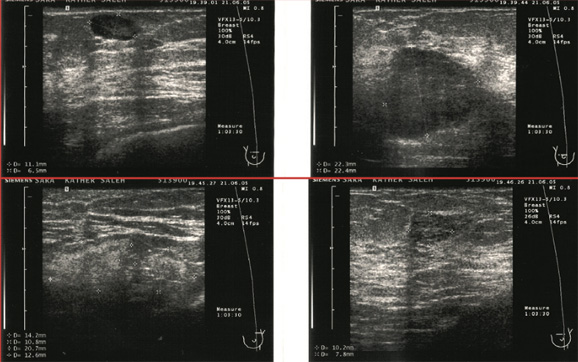
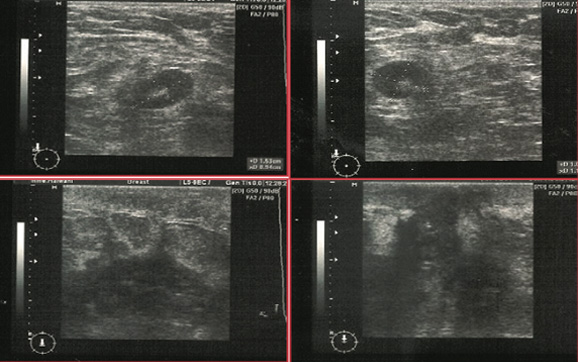
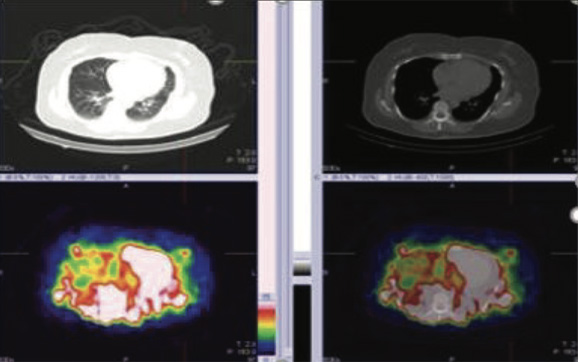
Case 3
USG BreastBilateral ductal dilatation ranging between 1.7 and 6.5 mm is seen. A fairly large fiboradenoma measuring 22.4*22.3 mm is seen lateral to Right nipple shadow.
One possible fibroadenoma measuring 10.2*7.8 mm is seen above the level of left nipple shadow.
One possible intra-mammary lymph node 11.1.*6.5 mm is seen superficially above and little lateral to the level of right nipple shadow. Multiple bilateral axillary lymph nodes are seen.
Case 3
SMM (Scintimammography)Focal areas of abnormally increased tracer uptake seen in
a) Larger one in upper quadrant of right breast.
b) Smaller one diagonally above the larger one in right breast (Lesion a is metabolically more active than b).
c) Upper quadrant of left breast, the tracer uptake intensity is much milder as compared to right breast abnormality (a) but looks like mirror image.
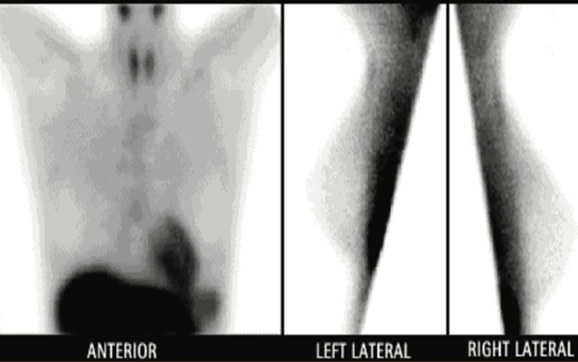
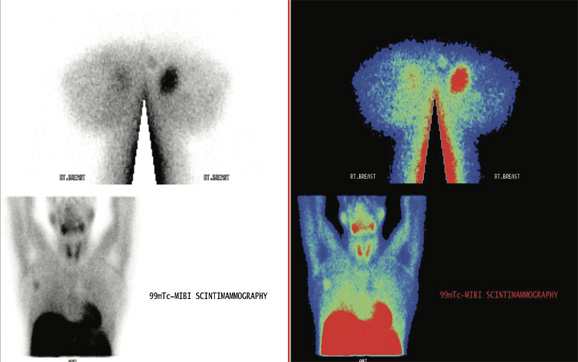
Case 4
Whole body 99mTc Sestamibi ScanSmall residual thyroid tissue in thyroidal bed and focal area of intense uptake in Left breast(Accidentally).
Breast Biopsy- Lobular breast cancer.
Case 5
SMM (Plannar Images)Focal area of abnormal MIBI tracer accumulation seen in both the breasts.
BFNAC Breasts - CancerousS cells are seen in boith the breasts.
Case 5
SMM (SEPCT-CT Fused Images Right Breast) Focal area of abnormal MIBI tracer accumulation seen in the right breast (axial images).
Case 5
SMM (SEPCT-CT Fused Images Left BreastFocal area of abnormal MIBI tracer accumulation seen in the left breast (axial images)
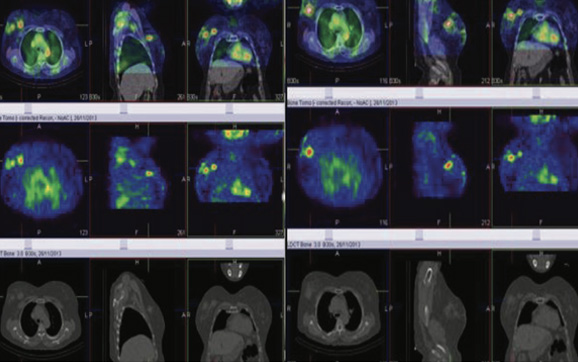
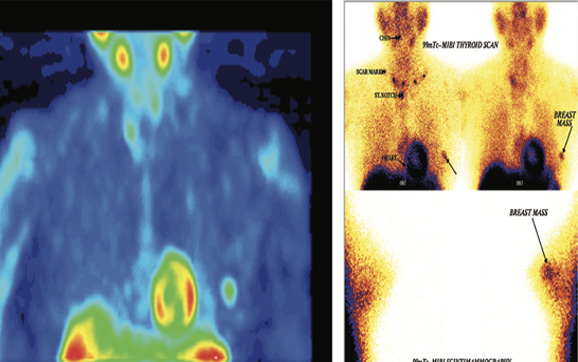
Case 6
MDP SMM (SEPCT-CT Fused Images)Multiple focal area of abnormal MDP tracer accumulation seen in the right breast (coronal views)

Case 6
99m Tc MDP Whole body scanBlood pool images shows focal area of abnormal MDP accumulation in right breast.
Static whole body bone images were unremarkable.
Case 7
99mTc-methoxyisobutylisonitrile scinti-mammography (SMM)Showing a typical case of breast cancer in the external upper quadrant of the left breast.