The skeleton is the second commonest site for metastases from prostate cancer after lymph nodes, and there is an incidence of 65–75 % of skeletal involvement in patients with advanced disease. Skeletal metastases are associated with significant morbidity and skeletal related events; however, effective palliation strategies are available resulting in improvements in overall survival.
Human skeleton is a living active organ that changes during normal physiological process of growth, remodeling, and in response to various pathological processes. Any process which interferes in the constantly changing dynamics of osteoclastic resorption and osteoblastic formation of bone results in various pathological and structural abnormalities. Nowadays, a number of structural and functional imaging modalities such as radiographs, computed axial tomography, magnetic resonance imaging, and hybrid SPEC CT bone scintigraphy with varying levels of sensitivity and specificity are employed to detect such abnormalities.
Radiographs can detect a change in skeletal lesion when it has progressed to about 50% change in bone mineralization. On the other hand, even a 5% change in osteoblastic turnover can be detected by technetium 99m (Tc99m) methylene diphosphonate (MDP) bone scintigraphy with its sensitivity being between 80% and 100% depending on the site of lesion and type of cancer.
Thus, radiographs have a limited sensitivity as compared to Tc99m MDP bone scintigraphy in detecting an early bony lesion. With the development of hybrid SPEC-CT (single-photon emission computed tomography combined with computed tomography) has improved detection sensitivity and specificity further.
Metastases on a bone scan can appear in different patterns. They may present either as a solitary or multiple foci or diffusely increased tracer uptake throughout the skeletal system.
A bone scan which demonstrates Intense & diffusely or heterogeneously increased tracer uptake throughout the skeleton system with markedly diminished or no renal activity (absent kidney sign) and excellent bone details with poor soft tissue uptake is known as super scan. Faint renal uptake was defined as an undoubtedly diminished renal activity compared with rib activity on visual inspection”
The mechanism most likely responsible for super scan appearance is diffuse reactive bone formation. This could be either due to diffuse metastatic disease or a generalized metabolic disease such as hyperparathyroidism. Because of increased uptake in skeletal system, the soft tissue uptake of radioisotope is very less, which results in increased skeleton to soft tissue activity ratio. Depending upon the degree of reactive bone formation, renal and bladder activity is faint or absent. The normal skeletal to renal ratio of absorption: isotope is 40%:60%. In cases of super scan, this ratio can be altered to up to 86%:14%.
Certain types of metastatic cancers such as prostate cancer, breast cancer, and lung cancer; metabolic bone disease such as renal osteodystrophy, Paget's disease, and hyperparathyroidism; hematological disease including leukemia, lymphoma, Wald Enstrom’s disease, and myeloproliferative disease and some miscellaneous conditions such as hyperthyroidism, fibrous dysplasia, intracranial glioma, hypervitaminosis D and systemic macrocytosis may show a super scan appearance on bone scintigraphy.
Pattern of uptake in super scan due to metastatic disease is different from that of metabolic disease. In metastatic disease, pattern of uptake is diffuse or there is heterogeneous uptake or patchy distribution of radiotracer in axial skeleton. In case of metabolic bone disease, uptake is more uniform in appearance, extends to distal appendicular skeleton and intense calvaria uptake that is disproportionate to the remainder of skeleton.
70 years old gentleman with history of generalized whole-body pain since last three months.
PSA- >100 ng/ml <4.0
MRI pelvis-Grade one prostatomegaly with heterogenous parenchymal signal and enhancement, median lobe indentation to the urinary bladder. Multiple enlarged pelvic and para-aortic soft tissues and lymph nodes. Multiple hypo and hyperintense bony lesions. Right ischium showed cortical thickening abnormal marrow signal and heterogenous enhancement. DD Paget, primary/sec bone tumor and others.
Adenocarcinoma of prostate, Gleason’s score 4+3= 7/10
About 80% of tissue (left and right) shows malignant features. Perineural invasion is seen in left lobe biopsy.
It revealed intense heterogeneous radiotracer uptake involving almost entire skeleton with high bone to soft tissue uptakes along with skull and mastoid bone. Bilateral kidneys were almost invisible.
These findings are suggestive of ‘metastatic super scan’
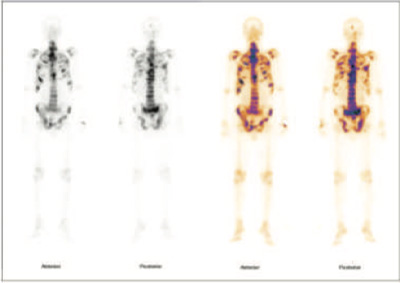
99mTc MDP whole body bone images
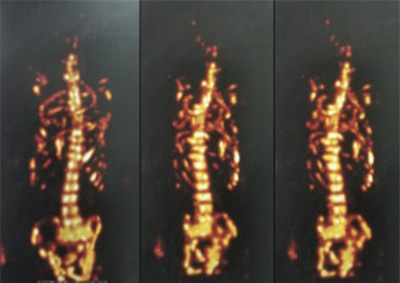
99mTc MDP Whole body bone 3D images
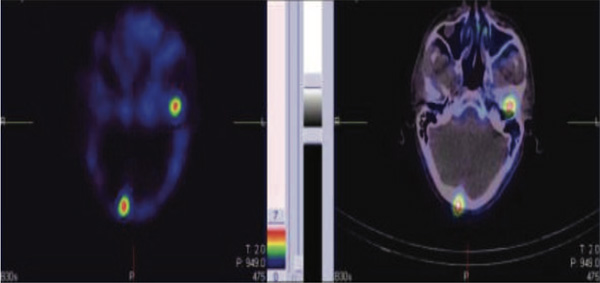
99mTc MDP hybrid SPECT-CT images of the bones
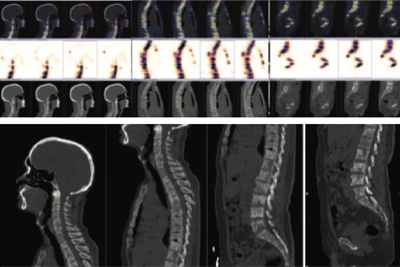
Underlying CT images shows mixed lytic & sclerotic throughout the skeletal system
Presence of a super scan usually indicates advanced stage of the disease, when there has already been extensive skeletal metastasis followed by an osteoblastic reaction. The patient prognosis is usually poor.
The overall incidence of super scan in different type of cancers was 1.3%, and in patients with underlying malignancy super scan appearance was most seen in prostate cancer followed by the breast and lung cancer The incidence of super scan appearance in prostatic cancer patients was 14.9%.
The bone scan continues to be recommended for the staging of skeletal metastases from prostate cancer. The development of hybrid SPECT CT (single-photon emission computed tomography combined with computed tomography) has improved detection sensitivity and specificity.