When you have a blocked tear duct, your tears can't drain normally, leaving you with a watery, irritated eye. The condition is caused by a partial or complete obstruction in the tear drainage system. A blocked tear duct is common in newborns. The condition usually gets better without any treatment during the first year of life. In adults a blocked tear duct may be due to an injury, an infection or a tumor. A blocked tear duct is almost always correctable. Treatment depends on the cause of the blockage and the age of the affected person.
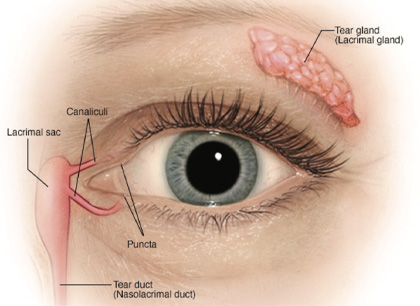
The lacrimal glands produce most of your tears. These glands are located inside the upper lids above each eye. Normally, tears flow from the lacrimal glands over the surface of your eye. Tears drain into the puncta, located in the inside corners of your upper and lower eyelids.
Your eyelids have small canals (canaliculi) that move tears to a sac where the lids are attached to the side of the nose (lacrimal sac). From there tears travel down a duct (the nasolacrimal duct) draining into your nose. Once in the nose, tears are reabsorbed.
A blockage can occur at any point in the tear drainage system, from the puncta to your nose. When that happens, your tears don't drain properly, giving you watery eyes and increasing your risk of eye infections and inflammation.
Signs and symptoms of a blocked tear duct include:
Blocked tear ducts can happen at any age. They may even be present at birth (congenital). Causes include:
Tears aren't draining the way they should, the tears that remain in the drainage system become stagnant. This promotes growth of bacteria, viruses and fungi, which can lead to recurrent eye infections and inflammation.
Any part of the tear drainage system, including the clear membrane over your eye surface (conjunctiva), can become infected or inflamed because of a blocked tear duct.
44 years old lady with history of recurrent right eye infection (conjunctivitis) each year since long (2010). Complaining of right watery eye and nasal blockage since last five months. Underwent nasolacrimal intubation but no obvious relief and hence referred for ENT work up, which was unremarkable.
Referred of Lacrimal Duct Scintigraphy (Dacryocystography)
9m Technetium Pertechnetate Dacryocystography
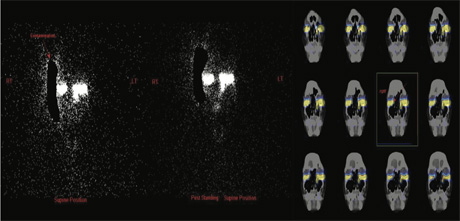
Dynamic images of both eyes were obtained in anterior supine position for the period of 40 minutes and subsequently static images are obtained at 45 min and SPECT-CT fused images at 120 minutes
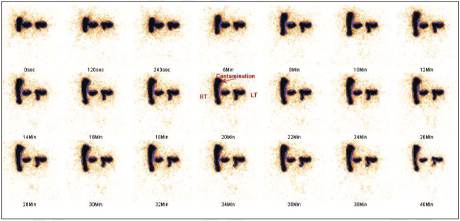
Left eye shows physiological tracer excretion into nasal cavity with well visualization of whole of the lacrimal duct.
Right eye shows physiological obstructive flow pattern at the level of punctum (As shown with arrow on SPECT-CT FUSED images).
The diagnosis of a right eye punctum stenosis was made.
Left eye shows physiological tracer excretion into nasal cavity with well visualization of whole of the lacrimal duct.
Right eye shows physiological obstructive flow pattern at the level of punctum (As shown with arrow on SPECT-CT FUSED images).
The diagnosis of a right eye punctum stenosis was made.
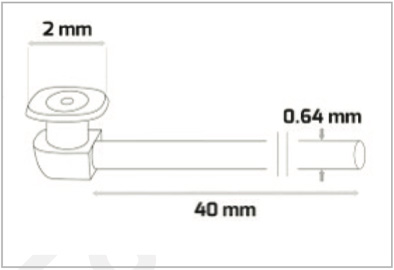
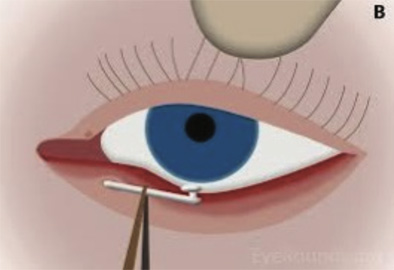
A 3-snip punctum opening was performed and a mini-Monaco tube was intubated to keep the punctum open and allow the tear to enter the lacrimal canal and thus her epiphora is controlled.
Lacrimal scintigraphy evaluates the lacrimal drainage apparatus in a “physiological” manner, that is, with pressure gradients present in every-day life; thus, it may be more suitable for the study of functional epiphora than other imaging modalities.