Epiphora is a bothersome clinical situation encountered in ophthalmology, which may necessitate significant diagnostic effort to be fully evaluated. The physician addressing this condition may rely on history or clinical signs to determine the causes, which may include lacrimal hypersecretion, canalicular (pre-sac) obstructions or stenoses, nasolacrimal (post-sac) obstructions or stenoses, or may even be functional (nonanatomic), due to a “lacrimal pump” failure. However, clinical information per se may not be enough and in that case, imaging modalities, such as lacrimal scintigraphy, may be required.
Lacrimal clearance (i.e., the elimination of tears from the conjunctival cul-de-sac) relies on several factors, such as gravity, capillary attraction forces, evaporation, absorption by the conjunctival surface, residual flow and the lacrimal “pump.
(performed by probing and injection or radio-opaque material into the canalicular system) may be adequate for the anatomical identification of stenotic sites but suffers from the fact that forced injection overcomes partial obstruction or stenosis.
Dacryoscintigraphy is an easy to perform, noninvasive Nuclear Medicine procedure and the functional integrity of the lacrimal drainage system can be assessed by visualizing the clearance of a small volume of radiopharmaceutical placed in the conjunctival sac into the lacrimal sac, duct and nasal cavity.
With the recent emphasis on minimally invasive management of patients with epiphora using silicone tube intubation and balloon dilatation, the physiological information provided by DACRYOSCINTIGRAPHY may be increasingly more useful in clinical decision-making process including appropriate patient selection and management.
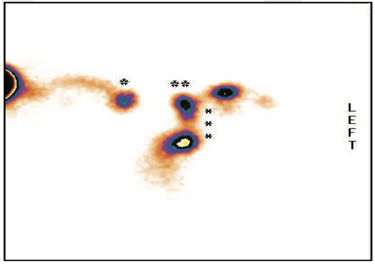
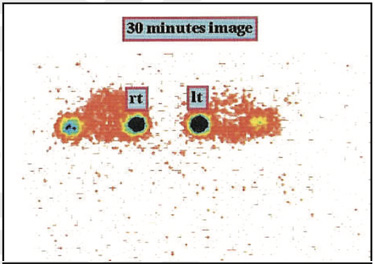
History of bilateral epiphora (right >left) with suspected lacrimal duct obstruction 99mTc-Dacryocystography- Left eye-showing physiological tracer excretion into nasal cavity around eight minutes onwards with well visualization of the lacrimal duct (Better appreciated in 30/60 min and SPECT-CT fused images as shown in figure 3)
Right eye shows slow physiological tracer accumulation in lacrimal sac and lacrimal duct with tracer hold up approximately at mid portion level of lacrimal duct (better appreciated in 30/60 min and SPECT-CT fused images as shown in figure 3) suggesting obstructive flow pattern approximately at the level of mid portion of the lacrimal duct.
Unilateral obstruction (right) at the level of common canaliculus & lacrimal Sac (as shown in figure).
Bilateral obstruction at the level of common canaliculus & lacrimal sac (as shown in figure).
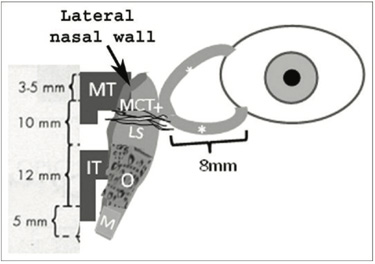
Case 1: Schematic anatomical presentation of the lacrimal drainage route, including the superior and inferior canaliculi (*), common canaliculus (+), lacrimal sac (LS), osseous (O) and membranous (M) parts of the nasolacrimal duct and middle and inferior turbinate's (MT and IT, respectively). The anterior part of the medial canthal tendon (MCT), the lateral nasal wall and the mean lengths (mm) of the above mentioned structures are also shown.
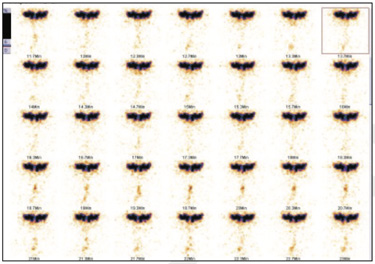
Fig. 1: Dynamic DRC images
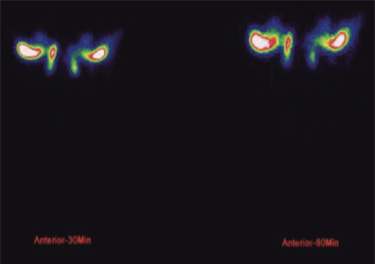
Fig. 2: static 30 & 60 minutes DRC images
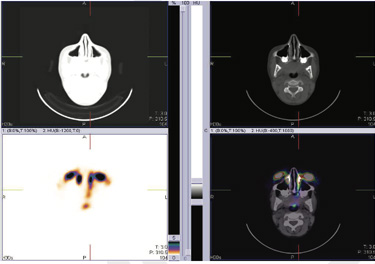
Fig 3 SPECT-CT FUSED DRC images 99mTc-Dacryocystography- Left eye shows physiological tracer excretion into nasal cavity around eight minutes onwards with well visualization of the lacrimal duct (better appreciated in 30/60 min and SPECT-CT fused images) Right eye shows slow physiological tracer accumulation in lacrimal sac and lacrimal duct with tracer hold up approximately at mid portion level of lacrimal duct (better appreciated in 30/60 min and SPECT-CT fused images) suggesting obstructive flow pattern approximately at the level of mid portion of the lacrimal duct.
Case 2Unilateral obstruction (right) at the level of common canaliculus & lacrimal Sac.
Case 3Bilateral obstruction at the level of common canaliculus & lacrimal sac.
Lacrimal scintigraphy evaluates the lacrimal drainage apparatus in a “physiological” manner, that is, with pressure gradients present in every-day life; thus, it may be more suitable for the study of functional epiphora than other imaging modalities.